Researchers at the University of Massachusetts and Massachusetts Institute of Technology (MIT) have successfully built a tissue-like bioelectronic mesh system integrated with an array of graphene sensors that can simultaneously measure both the electrical signal and the physical movement of cells in lab-grown human cardiac tissue.
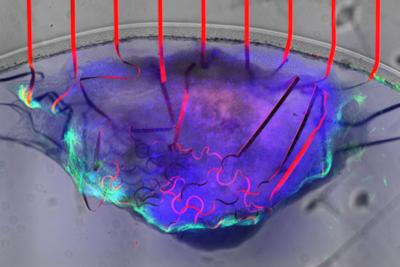
A bioelectronic mesh, studded with graphene sensors (red), can measure the electrical signal and movement of cardiac tissue (purple and green) at the same time. Image credit: UMass Amherst
The tissue-like mesh can grow along with the cardiac cells, allowing researchers to observe how the heart’s mechanical and electrical functions change during the developmental process. The new device can be extremely useful for those studying cardiac disease as well as those studying the potentially toxic side-effects of many common drug therapies.
Cardiac disease is the leading cause of human morbidity and mortality across the world. The heart is also very sensitive to therapeutic drugs, and the pharmaceutical industry spends millions of dollars in testing to make sure that its products are safe. However, ways to effectively monitor living cardiac tissue are extremely limited. In part, this is because it is very risky to implant sensors in a living heart, but also because the heart is a complex muscle with more than one thing that needs monitoring. “Cardiac tissue is very special,” says Jun Yao, associate professor of electrical and computer engineering in UMass Amherst’s College of Engineering and the paper’s senior author. “It has a mechanical activity—the contractions and relaxations that pump blood through our body—coupled to an electrical signal that controls that activity.”
But today’s sensors can typically only measure one characteristic at a time, and a two-sensor device that could measure both charge and movement would be so bulky as to impede the cardiac tissue’s function. Until now, there was no single sensor capable of measuring the heart’s dual properties without interfering with its functioning.
The new device is made of two critical components, explains lead author Hongyan Gao from UMass Amherst. The first is a three-dimensional cardiac microtissue (CMT), grown in a lab from human stem cells under the guidance of co-author Yubing Sun, associate professor of mechanical and industrial engineering at UMass Amherst. CMT has become the preferred model for in vitro testing because it is the closest analog yet to a full-size, living human heart. However, because CMT is grown in a test tube, it has to mature, a process that takes time and can be easily disrupted by a clumsy sensor.
The second critical component involves graphene— which has a few surprising quirks to its nature that make it perfect for a cardiac sensor. Graphene is electrically conductive, and so it can sense the electrical charges shooting through cardiac tissue. It is also piezoresistive, which means that as it is stretched—say, by the beating of a heart—its electrical resistance increases. And because graphene is extremely thin, it can register even the tiniest flutter of muscle contraction or relaxation and can do so without impeding the heart’s function, all through the maturation process. Co-author Jing Kong, professor of electrical engineering at MIT, and her group supplied the graphene material.
Gao, Yao and their colleagues then embedded a series of graphene sensors in a soft, stretchable porous mesh scaffold they developed that has close structural and mechanical properties to human tissue and which can be applied non-invasively to cardiac tissue.
“No one has ever done this before,” says Gao. “Graphene can survive in a biological environment without degrading for a very long time and not lose its conductivity, so we can monitor the CMT across its entire maturation process.”
“This is crucial for a number of reasons,” adds Yao. “Our sensor can give real-time feedback to scientists and drug researchers, and it can do so in a cost-effective way. We take pride in using the insights of electrical engineering to help build tools that can be useful to a wide range of researchers.”
In the future, Gao says, he hopes to be able to adapt his sensor to grander scales, even to in vivo monitoring, which would provide the best-possible data to help solve cardiac disease.